The Tree That Could Help Stop the Pandemic
In early april, Paul Hiley was kicking back in the executive suite at Desert King International LLC, gazing out the window at the San Diego sunshine and daydreaming about his golf game. California had issued its initial stay-at-home order for COVID-19, but apart from the hand sanitizer around the office, life was more or less normal. Retirement was on the horizon for Hiley. Maybe he’d sell the business. Maybe his son, Damian, would take over.
For more than 42 years, Hiley has been a leading purveyor of certain plant-based food additives such as saponins, foaming agents used in root beer and Slurpees. Most of us never think about these compounds, and Hiley has always liked it that way. “My theory of business is the only two people who need to know my name are my wife and my banker,” he told me recently.
Then, one day—April 14th, to be exact—his son told him that they had a call with Stanley Erck. Erck is the CEO of Novavax, a Maryland-based maker of vaccines. Not a seller of vaccines, mind you: The company had yet to bring one of its candidates to market. But like other companies around the world, Novavax had thrown its hat into the coronavirus-vaccine race. And its success, Erck believed, depended on that odd ingredient in Slurpees.
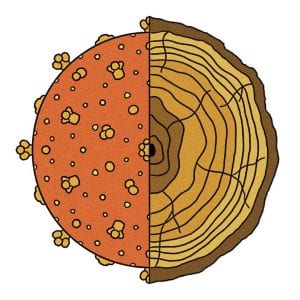
The inner bark of the Chilean soapbark tree, Quillaja saponaria, is the source material for some of these saponins. Pulverized and soaked in water at the Desert King factory in Chile, the bark is transformed into a brown, bitter, bubbly fluid. This precious goo does many things well, and it happens to be the raw material for one of the world’s most coveted vaccine adjuvants: QS-21. Adjuvants are compounds that boost the body’s immune reaction to a vaccine. Owing to their potential risks to human health, however, only a handful of adjuvants have been approved by the U.S. Food and Drug Administration, and QS-21 is one of the newest.
A single gram of powdered QS-21 costs more than $100,000, though only about $5 worth is needed for each shot. Nine years ago, researchers estimated that the global supply of pharmaceutical-grade Quillaja extract was sufficient for just 6 million doses of vaccine. Everyone in the business knew the story of the Pacific yew tree, whose bark was the original source of the chemotherapy drug paclitaxel, and which was threatened by large-scale harvesting in the 1980s. “If you take out all the trees in one shot and deplete the source of saponin, you are in deep shit in the future,” says Garo Armen, whose company, Agenus, helped bring QS-21 to market. Novavax has its own saponin-based adjuvant, called Matrix-M, and warned investors last year that their vaccines could be delayed if they failed to “secure sufficient supplies” of high-quality extract. And the Hileys practically had a monopoly on it.
During his call with the Hileys, Erck asked if Desert King could increase their production for Novavax a hundredfold. Paul Hiley’s jaw dropped to the table. Novavax was on the cusp of receiving $384 million in international funding to help it produce 100 million doses of its COVID-19 vaccine for the world by the end of the year, and a billion doses by the end of 2021. It would also soon be on the short list of vaccine candidates funded by the Trump administration’s Operation Warp Speed. Novavax needed guarantees of 1,500 pounds of saponin now, and up to three times as much next year.
Hiley’s immediate concern was that his Chilean operation had already missed the bark-harvesting window—typically during the trees’ spring growth, between September and December. And last year he had made the ill-timed decision to postpone expanding their pharmaceutical operations in favor of investing in Desert King’s booming animal-feed business.
In the end, Hiley knew there was only one way to answer Erck: “Of course, we can deliver it,” he said. Three months later, inside the Desert King conference room in early July, sitting across from a shelf displaying Slurpee cups and bottles of Stewart’s Root Beer, Hiley let out a chuckle through his surgical mask. “I had no idea if we could.”
For all the talk about the cutting-edge vaccines that may just get us out of the COVID-19 mess, little has been written about adjuvants. Perhaps that shouldn’t be surprising: The late Yale professor Charles Janeway famously called adjuvants the “immunologist’s dirty little secret.”
These unheralded helpers can turn a half-baked vaccine into an effective one, or stretch a scarce vaccine supply during a pandemic. Not every vaccine requires an adjuvant, but many do: Of the more than 200 vaccines listed in the Milken Institute’s COVID-19 vaccine tracker, approximately 40 percent are protein-based vaccines, which rarely work without an adjuvant. Yet adjuvants have never attracted much funding from industry and government. “Adjuvants have been the weak link in vaccines for the last hundred years,” says Nikolai Petrovsky, a vaccine researcher at Flinders University in Adelaide, Australia.
The discovery of adjuvants is credited to a bearded veterinarian named Gaston Ramon, who worked at the Pasteur Institute in Paris in the 1920s. At the time, horses were routinely injected with toxins from tetanus and diphtheria so their bodies would produce antibodies that could be used in human therapies. Ramon, who was trying to develop the first human vaccines for these life-threatening diseases, observed that the horses’ circulating antibodies generally declined over time—even if the animals were re-injected with bacterial toxins every few weeks. Every so often, however, a new injection would cause waning antibody levels to rebound.
When he examined the horses whose antibody levels rebounded, Ramon discovered abscesses at their injection sites. Those pus-filled lumps, he thought, could be temporarily trapping the toxins, giving the horses’ immune systems more time to ramp up their responses. Ramon experimented with ways of artificially slowing the absorption of the injected toxins, mixing them with bread crumbs, powdered infant formula, and tapioca starch—which happens to contain high levels of saponins—to produce local swelling without a full-blown abscess. One horse in his study, injected with a mix of toxins and tapioca, produced five times the normal levels of antibodies.
Meanwhile, a British researcher found that aluminum salts, injected into guinea pigs, had similar but more predictable effects on antibody production. For the next 70 years, they would be the only adjuvants used in vaccines. (While aluminum adjuvants can produce swelling and pain that lasts for a few days, abscesses and other side effects are uncommon.)
The earliest viral vaccines actually did fine without adjuvants. The polio and measles vaccines were initially made from weakened or inactivated whole viruses, which were more than 90 percent effective after several doses. Both vaccine types generate an antibody response, and the live ones also activated another part of the immune system, the T-cell response, which is important for fighting more complex pathogens and can even kill the body’s own cells if they become infected.
The risk of live-virus vaccines is that they can possibly revert to their more dangerous selves or replicate uncontrollably in people with weakened immune systems. Inactivated-whole-virus vaccines have also raised alarm after episodes where they altered the immune system in unpredictable ways. During a clinical trial in the 1960s, 31 infants received a vaccine made with inactivated respiratory syncytial virus (RSV). Those who later caught the virus ended up with a more severe form of the disease; two of the 23 who were infected died. By the early 1980s, the quest for ever-safer vaccines against ever-trickier viruses, such as RSV, hepatitis B, and HIV, led researchers to develop vaccines that contained just a fragment of the virus, typically a protein.
But the immune system seemed blind to these new vaccines—until researchers added just the right adjuvant. Aluminum didn’t stimulate an appropriate T-cell response, which scientists noticed could be induced with other substances, such as heat-killed tuberculosis bacteria. “Why do we need to use adjuvants?” Janeway asked in 1989. “To be quite honest, the answer is not known.”
Adjuvants posed their own dangers. During a pilot study of an adjuvanted flu vaccine in the 1990s, some subjects got triple-digit fevers and egg-shaped lumps on their arms. “That scared people,” says Tyler Martin, who once worked at the Chiron Corporation, which developed that vaccine. Adjuvants became a frequent target for the anti-vaccination community, which contributed to the FDA’s conservative approach to them. “At advisory-committee meetings, people come out to rail against adjuvants,” Peter Marks, the director of the FDA’s Center for Biologics Evaluation and Research, says. “We want to make sure they are safe.”
In any event, the side effects were proof that adjuvants weren’t simply slowing down the spread of the antigen through the body. Perhaps, as Janeway himself theorized, they were flipping on some ancient danger switch to alert our immune system of an invader. In 1997, scientists located that switch: Our dendritic cells—the tentacled sentries lurking in our tissues—have at least 10 receptors attuned to pathogens. Some adjuvants act on those receptors. Martin, now the CEO of Adjuvance Technologies in Lincoln, Nebraska, told me, “Once we understand what’s the nature of the immune response we really want to create to COVID, then we can pick the right adjuvants to sculpt that response.”
Acouple of weeks after meeting the Hileys, I stood across the street from a Starbucks on the wooded edge of the University of California at Berkeley. It was 10 o’clock on a Wednesday morning in mid-July, but the place was uncannily quiet—all summer classes had moved online. During the previous week, the county had reported more than 1,000 new cases of COVID-19, the highest totals since the outbreak began.
After a few minutes, a man rolled up on his bicycle, a buff cinched around his nose and mouth. Intense dark eyes peeked out from under his fluorescent-green helmet. This was Ricardo San Martin, a scientist who had helped develop the Chilean soapbark industry. He had moved on to other projects, but he still consulted for Desert King. In April, he said, he got a WhatsApp message from Damian Hiley that said simply: “Google Novavax.”
When San Martin heard that Novavax was going to need several thousand pounds of Quillaja extract each year, he started doing the calculations in his head. Since 2000, Chile has cleared 11 percent of its native forests, and mature, accessible Quillaja saponaria trees have become rare. Under Chilean law, landowners need a special permit to cut down Quillaja trees, but they are allowed to prune up to 35 percent of their biomass every five years. Over the next few years, the industry was on course to exceed one published estimate of the maximum sustainable harvest of 27,000 tons, or about 67,500 trees. The Hileys say that number is a significant underestimate of what the forests can bear. Regardless, just one major vaccine rollout would require bark from the equivalent of 5,000 to 7,000 trees per year—or more if you’re only relying on prunings. San Martin realized that while most of the world was thinking about the pandemic’s risk to the human species, someone needed to be thinking about its antidote’s risk to Quillaja. “I feel like if I don’t do it,” he told me, “then who’s going to do it?”
Keeping a safe distance from each other, San Martin and I walked around the perimeter of a small grove of trees just within the campus boundary, mostly eucalyptus and redwoods. We came to a tree about 60 feet tall with gray, sandpapery bark and waxy, oval-shaped leaves with rippled margins. This was it: a Chilean soapbark, one of a handful planted on the Berkeley campus starting in the late 1800s. San Martin—a chemical engineer, not a botanist—doesn’t know how they all ended up here, just that he’s lucky to live near them. (The soapbark is uncommon in the United States and tends to grow well only in California, which has a climate similar to Chile’s.)
Pulling a pair of garden clippers out of a pannier on the side of his bike, he snipped off a few leafy branches to tuck inside a paper bag. Later, back in his garage laboratory a few blocks from campus, San Martin ground up the dried leaves and soaked them in warm water to produce an extract. As he shook the liquid up in a large graduated cylinder that looked like a theater prop, counting to 30, it produced a dense foam like the head of a beer. The amount of that foam, he explained, was roughly equivalent to the extract’s saponin content.
 Melanie Lambrick
Melanie Lambrick
Leaves aren’t currently used by industry because they represent just 5 percent of a mature tree’s weight. In a sapling, however, they may account for 30 to 50 percent of the tree’s biomass and are the only material that can be harvested sustainably. In the face of the current public-health emergency and the potentially life-saving role of saponin adjuvants, San Martin believes we should be establishing new soapbark-tree plantations inside and outside of Chile, and preparing to harvest leaves from the young trees. He’s now testing local soapbark stock inside Berkeley’s greenhouses, hunting for the plants best suited to found plantations on American soil. “What I want now, urgently, is to provide a second source of this natural raw material,” he said.
He hopes to finish a mission he began long ago.
Flash back to the early 1990s: Picture, if you will, San Martin sitting on the toilet. He was a newly minted Ph.D., working at the Catholic University in the Chilean capital of Santiago. He was looking for a project with commercial potential, something that might contribute to the Chilean economy as the country recovered from the cruelty and corruption of the Pinochet dictatorship. He had brought a copy of a United Nations newsletter into the bathroom, and one article caught his eye. It said that a “South American tree” was being tested in a vaccine against HIV.
Only later did he realize that one of those very trees was growing in his own backyard. Chilean soapbarks were once abundant in the sun-soaked hills around the capital, climbing up the flanks of the Andes to about 6,000 feet. For hundreds, if not thousands, of years, the tree bark, ground up and mixed with water, was used as soap by the indigenous Mapuche people. In his 1782 treatise on the natural history of Chile, the Jesuit priest Juan Ignacio Molina wrote of its use by locals: “There is never to be seen on their clothes the least spot or dirt.”
Over the next century, soapbark became an international commodity. American magazines offered up recipes for hair-curling liquids and wool detergents made with the soap-like saponins. Sozodont toothpaste advertised itself as “the only dentifrice” that contained “this salubrious botanical product.” (“When rosy lips part, pearls should glitter behind them.”) In the early 1900s, makers of carbonated beverages discovered that adding soapbark extract to their drinks created a coating of bubbles on the surface that kept the carbonation from escaping. From there, the applications of saponin expanded rapidly: During World War II, it was used in surveillance efforts as both a lens cleaner and an ingredient in photographic reagents.
In 1949, a U.S. government report noted that careless bark-stripping methods were destroying “thousands of trees each year” and regulations were poorly enforced. Some harvesters simply peeled off the vital bark from around the main trunk, girdling the trees and leaving behind a slowly dying forest. Felling 25-year-old trees for about 35 pounds of bark was also wasteful: Up to 95 percent of their weight was being left to rot in the field. Landowners were paid just $30 for a tree’s worth of bark, which was then sent overseas for processing. Chile was destroying its natural heritage for a pittance, and when San Martin met with forestry experts, they asked if there was anything he could do to help.
Back in his lab, San Martin began to study the chemical makeup of the tree’s fibers. Although saponins are most abundant in, and easiest to extract from, the bark, he found he could also obtain them from the trunk and the branches. Using this method, a single tree could replace five or six destroyed in the past. He also found that through judicious pruning, one could improve the condition of the scraggly stump-sprout trees left behind from previous clearcutting.
San Martin hoped to develop a soapbark-processing industry in Chile, and he set out to find international buyers for saponin. With the help of a university loan, he started a company called Natural Response and spent several years hunting for customers—with little luck. With three kids to support, his bank account was shrinking, and interest on the loan was piling up. “I had one car from 1970-something with no brakes,” San Martin said. “I was bankrupted, honestly.”
In 1995, one of San Martin’s employees sent a fax to Paul Hiley, whose business at that time revolved around saponins from Mexican yucca. Within days, Hiley was stepping off a plane in Chile. San Martin took him to the university to show him a small barrel of highly purified, powdered white saponin. “He was proud of his little production facility,” Hiley told me.
But Hiley wasn’t interested in the high-grade stuff back then. He pointed at the cola-colored syrup that San Martin had yet to process. The crude extract was exactly what Hiley needed for his clients in the soft-drink business. “I’ll buy 10 tons,” Hiley said. He purchased that first shipment and then wired San Martin an extra $300,000 to partner with him and expand the business.
San Martin was still in a hole: He needed his extract to be a pure liquid, but it came out cloudy, filled with microscopic particles. Every attempt to refine it in the factory negated the cost-saving efficiencies he’d achieved in the field, and he wasn’t hitting the price targets he had promised Hiley. “I couldn’t say, ‘Paul, pay me 12, and you sell it at 11.’”
In the late 1990s, while visiting his children in Montpellier, France, he stopped in a bookstore. He plucked a two-volume treatise on wine making off the shelf. “Why did I pull that out? I don’t know,” San Martin said. As he started reading, he realized that the food-safe processes that vintners used to remove clumps of tannin from their fermented grape juice could be applied to soapbark extract: “I rushed to Chile with that thing.” It was his Eureka moment.
It was also his introduction to the Jevons paradox, the frustrating phenomenon by which technological increases in efficiency fuel increased demand. With San Martin’s innovations, the annual harvest of Quillaja declined from a high of 20,000 tons per year to around 5,000 tons. Then it started creeping up, exceeding 11,000 tons in 2012. The annual harvest is now approaching 20,000 tons again, according to Hiley.
To some degree, this was San Martin’s own fault. He couldn’t stop inventing new applications for the soapy substance. He discovered that it could be used as a bio-pesticide for nematodes on grapes. (Saponins likely evolved as a defense against pests.) Then he found that it reduced the toxic mist of sulphuric acid that rises out of copper-extraction tanks.
San Martin sold his remaining stake in the business to Hiley in 2005, and moved to Berkeley in 2013. Over the past 15 years, the fastest-growing part of Desert King’s business has been their saponin-based animal supplements, which can improve growth rates and reduce Salmonella infections in chickens. Desert King says its saponins, manufactured and sold by major feed companies, are now fed to more than 50 percent of antibiotic-free poultry in the U.S. The supplements are also showing promise in preventing infections of viruses and parasites in fish, including farmed salmon, a big business in Chile.
Everyone at Desert King was enough of a believer in Quillaja’s juju that they began putting a few drops of extract into their coffee or orange juice each day to ward off disease. “It tastes like soap,” Damian Hiley told me. Whether this did anything for their health was doubtful, but the profits were undeniable: By the late 2000s, the company was bringing in tens of millions of dollars per year. Then, three years ago, the Food and Drug Administration gave QS-21 the nod of approval. “Everyone was knocking on our door,” Damian said.
It is often said that vaccines are one of the most successful public-health interventions in human history. They are also bad business propositions. Two-thirds of vaccines fail in clinical trials. Once approved, they are often less profitable than drugs for cancer or rare diseases. In 2004, just five companies were manufacturing vaccines for Americans, down from 26 in 1967.
Since then, vaccine makers have lost money trying to develop vaccines for Zika and Ebola, because the outbreaks subsided and government funding dried up. When the new coronavirus landed on U.S. shores, the major vaccine makers sat on the sidelines for weeks—a situation that Anthony Fauci, the director of the National Institute of Allergy and Infectious Diseases, characterized as “very frustrating” during a February event at the Aspen Institute.
Novavax, however, was the eager kid waving a hand in the back of the room. Founded in 1987, the company had so far failed to bring a vaccine to market, and stayed afloat through private investment, research contracts, and licensing deals. Last year, its clinical trial for an RSV vaccine was a bust. Tens of millions of dollars went down the drain, employees were laid off, and two development and manufacturing facilities were sold. Soul searching ensued. “If you get bad data, everybody thinks you’re a failure,” Gregory Glenn, the company’s president of R&D, says. “I have PTSD from that.”
They got a gold star for attendance, though. Over the past decade, Glenn’s scientists have repeatedly pursued vaccines for emerging diseases including swine flu, Ebola, and Middle East respiratory syndrome, another coronavirus. Their laboratories maintained a stock of cells originally plucked from the ovaries of caterpillars in the 1970s. These cells were little factories that could be induced to pump out just about any kind of virus protein, including the coronavirus spike.
Before Glenn joined Novavax in 2010, the company wasn’t a believer in adjuvants, arguing that an unadjuvanted flu vaccine would be faster to win FDA approval. But Glenn, a pediatrician who had worked in the laboratory of an adjuvant expert at the Walter Reed Army Institute of Research, thought it was time to embrace them.
Adjuvants had undergone a renaissance, and QS-21 was its poster child. A crude saponin extract had been used in veterinary vaccines since the 1950s, but it was too toxic for humans, causing red blood cells to burst. In the 1990s, a researcher named Charlotte Kensil separated some of the 50 or so saponins in Quillaja saponaria extract, then tested them individually in mice. QS-7 was a potent adjuvant, but there wasn’t a lot of it. QS-18 proved to be the most toxic. QS-21 was relatively mild and generated both an antibody and a T-cell response.
GlaxoSmithKline licensed QS-21 from the maker. In order to tune the immune response, it combined QS-21 with a second adjuvant, a fat-like substance derived from Salmonella bacteria. Three years ago, this potent combo came onto the market in their shingles vaccine, called Shingrix. “That vaccine hit the ball out of the park,” says Janet McElhaney, an expert on aging and immunity at Health Sciences North in Ontario.
Shingrix conferred immunity on 91 percent of people over 70 years old, more than double that of a previous shingles vaccine. Last year, the same adjuvant combo was rolled out in parts of the world in GSK’s malaria vaccine, Mosquirix, and it is also a component of a late-stage-tuberculosis vaccine candidate.
Novavax, meanwhile, obtained the rights to a different saponin-based adjuvant, now called Matrix-M, which was developed by a Swedish researcher who had worked on that HIV vaccine San Martin first read about. Recently, Novavax has tested Matrix-M as part of its NanoFlu vaccine, which not only provided a stronger antibody response than existing flu vaccines but also offered cross-protection against multiple strains of influenza.
By the time COVID-19 arrived, the company was finishing up Phase 3 clinical trials of NanoFlu, which would demonstrate Matrix-M’s safety in 2,650 human subjects. In February, it began testing its COVID-19 vaccine with Matrix-M in animals, and the results coming out in the spring were promising. “We all need to be humble in front of trying to make a billion doses,” Glenn told me a couple of months ago. “But, so far, things have gone exceptionally well for us.”
No matter how effective a COVID-19 vaccine is, it won’t put a dent in the pandemic unless it can be produced on a massive scale. The downside of an adjuvant is that it adds one more link to the global supply chain, one more crucial connection that can be broken. And by the time Novavax was preparing for its first human tests, the Hileys were struggling to keep their doors open.
As COVID-19 started to circulate in the U.S., Desert King had to provide van transportation for its 220 Chilean workers to replace the public buses forced out of service due to pandemic restrictions. The company pulled strings with local officials for lockdown waivers, and solicited letters of support from Coca-Cola and GSK. By the middle of May, however, they no longer had enough employees coming to work to run their boilers, and they had to shut down. “Every company had the same sob story,” Damian Hiley said. “Maybe our messaging was falling on deaf ears.”
The impending closure triggered a red alert at Novavax’s headquarters, some 5,000 miles away. The company sent an official letter to Chilean President Sebastián Piñera, requesting his assistance to help them put a halt to the pandemic. A couple of days later, Desert King got the exemption it needed and was cranking out Quillaja extract around the clock. It also resolved to break ground on a new pharmaceutical manufacturing suite. In July, Novavax made headlines with a $1.6 billion commitment from Operation Warp Speed, the largest award at the time.
The Hileys knew that their harvesting practices in Chile were now under the global microscope. During my visit to Desert King’s headquarters, Damian showed a brand-new company video that included drone photos of vast stands of Quillaja, an upbeat soundtrack, and the soothing voice of a female narrator describing the company’s “sustainable objectives” and “responsible management.”
“We hadn’t had to do this before,” he said of the public-relations campaign. “We really want to make sure that people understand, especially in Chile, that we are doing this in a responsible, sustainable, renewable, kosher, dotting-every-i-and-crossing-every-t way.”
“I’m not an environmentalist by any stretch,” his father added. “As a capitalist, which I am, if I can make a buck, honestly, legally, and help people and not damage Mother Earth, well, check, check, check.”
Desert King doesn’t own much land in Chile. Instead, they make agreements with local landowners. Their harvesters prune trees at intervals ranging from seven years to 20, using San Martin’s low-impact methods. They peel off all the bark they need for vaccines and use the rest of the tree biomass they harvest for their other businesses. They have mapped and tested thousands of trees to track their saponin makeup, which varies greatly by location. “Any fool can go to Chile and harvest a few trees,” Damian said. “The problem with QS-21 is that out of 100 trees, maybe five of them have the right profile.”
As part of its long-term growth plan, Desert King gives out seedlings to Chilean landowners and encourages them to plant native Quillaja instead of exotic eucalyptus and pine. The country’s forestry managers have also distributed Quillaja seedlings around the country—139,000 last year, more than any other species. Five years ago, Desert King invested in a plantation specifically for their pharmaceutical contracts, using cloned trees high in QS-21. Those trees are now large enough for harvesting, but the company still has to ensure that the adjuvant produced from their extract will be equivalent in makeup and quality to what they were using before.
Desert King plans to establish additional plantations in Chile, and possibly elsewhere, to match the needs of Novavax’s adjuvant, but any seedlings planted now will take years to produce harvestable bark—which is why San Martin’s work on Quillaja leaves is so critical. “Who knows what’s going to happen in Chile?” Damian said. “What if they say it’s illegal to harvest Quillaja?” The current supply is vulnerable in other ways: In January 2017, the country had the worst fires in its history, which burned more than a million acres of central-south Chile—a region home to Quillaja trees.
Such concerns have provided an opening for Desert King’s competitors. Tyler Martin of Adjuvance Technologies told me that they can increase the adjuvant yield from a tree by a factor of a hundred, using its semisynthetic version of QS-21. Meanwhile, Agenus is now working with another company to grow QS-21 inside vats filled with cultured plant cells. Its partner, Phyton Biotech, used this method to wean the world off the Pacific yew, and is now the world’s largest supplier of paclitaxel.
The other drugmakers partnering on a protein-subunit vaccine in Operation Warp Speed aren’t taking any chances with the saponin supply chain. GSK and Sanofi are using GSK’s less-potent oil-in-water adjuvant. It, too, contains a natural product—an oily compound from shark livers—but it is unlikely to face a supply constraint and has already been stockpiled. “That’s the way I would have gone,” Carl Alving, a retired Army adjuvant expert, says. “It’s much less expensive and much less difficult to formulate and put together in a very rapid period of time.”
Damian Hiley brushes off the suggestion that the world shouldn’t rely on Quillaja for a COVID-19 vaccine. “That’s complete bullshit,” he said. “There’s plenty of material.” What his naysayers don’t realize, he said, is that San Martin recently revamped their process of extracting saponin from bark, allowing the company to double its efficiency. The company also believes Chile’s forests can sustain four times the current annual harvest. If supplies become tight and saponins are needed for multiple vaccines, they’d just shift production away from, say, chicken feed. “Maybe one day,” he said, “we’ll have to say to those customers, ‘Sorry, guys, we’re no longer supplying this.’”
On august 4th, Novavax released the first data from its initial safety trials, which had tested the vaccine on 131 human subjects. The immune response was stellar, activating both antibody and T-cell production. “This is the first time I’m looking at something and saying, ‘Yeah, I’d take that,’” the Cornell virologist John Moore told The New York Times. As with other COVID-19 vaccines, some patients had experienced headaches, fatigue, and swelling at the injection site, but there were no serious side effects.
Novavax’s protein-based vaccine will likely only arrive on the U.S. market after the faster-to-develop RNA vaccines from Moderna Therapeutics and Pfizer have received emergency approval. But unlike those gene-based vaccines, which require ultra-low-temperature freezers, protein-based vaccines can be stored in refrigerators, simplifying global distribution. Novavax has entered Phase 3 trials in the United Kingdom, while interim data from their Phase 2 trial in the U.S. is expected by the end of the year. Japan, Canada, South Korea, and the United Kingdom have now secured purchase agreements with Novavax, and the company expects to be able to produce 2 billion doses of vaccine annually in 2021.
San Martin wants a safe, effective vaccine as much as anyone on Earth. While I was in Berkeley, he told me that two of his old friends from Chile had recently died from COVID-19. He and his wife had decided to temporarily increase their social-distancing measures. Six feet wasn’t far enough; he wanted 10.
He is looking forward to being able to have a beer with friends, listen to live music, and talk about old times with Paul Hiley without wearing a mask. At times, the thought crosses his mind that he’s the only person who can save the trees in Chile. He brushes such anxious thoughts aside, though, because they prevent him from focusing on the science.
As San Martin and I stood next to Berkeley’s soapbark trees, a groundskeeper rolled up behind us in a maintenance vehicle, a weed whacker and trash can in its bed. “What are we doing?” she hollered.
San Martin spun around, a bouquet of leaves in his hand. “I’m taking a sample,” he said. “This tree has some compounds that are now being used in the best candidates for the COVID vaccine.”
“Wow! That’s amazing,” the woman replied. “We’ll have to plant a lot of those, huh?”
We took a moment to laugh, and to appreciate a brief social connection in dark times. The woman zoomed away. San Martin turned back to the tree with a serious look in his eyes. He craned his neck up toward the drooping branches overhead, then back at the promising leaves in his hand. “Okay,” he said. “So, here we go.”
BRENDAN BORRELL is a Los Angeles–based writer. He is currently working on a book about the coronavirus-vaccine race.
Fuente: The Atlantic
